Diagnosis and Tests
How is a migraine diagnosed?
A healthcare provider will diagnose a migraine after a physical exam and neurological exam. They’ll also learn more about your medical history and biological family health history. Your provider may ask you questions to learn more about your symptoms, including:
- What symptoms do you experience?
- Can you describe the feeling and location of your headache?
- How severe are your symptoms?
- How long did your symptoms last?
- Did anything make your headache better or worse?
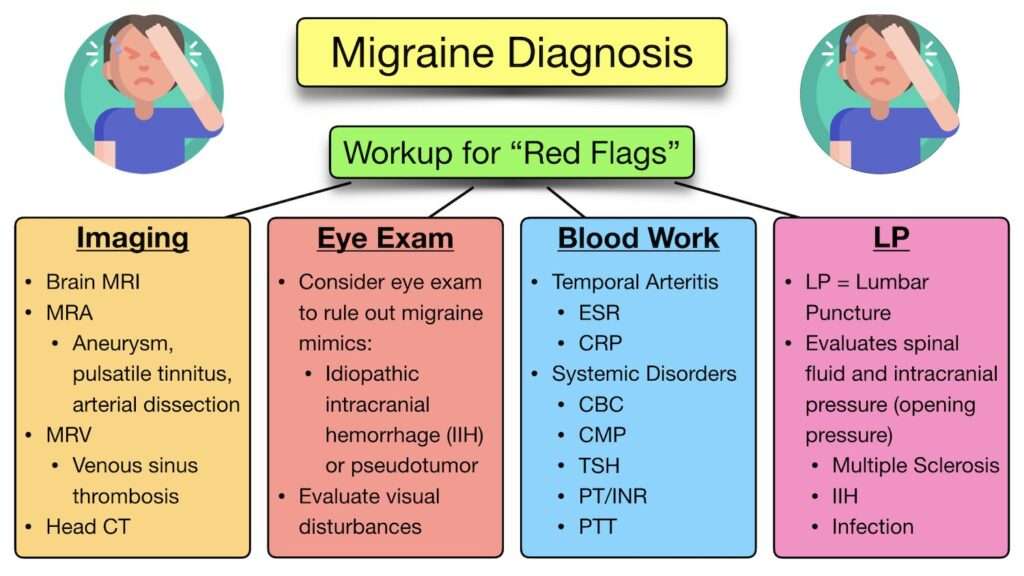
Your provider may also order blood tests and imaging tests (such as a CT scan or an MRI) to make sure there aren’t any other causes for your headache. An electroencephalogram (EEG) may help your provider rule out other conditions.
Management and Treatment
How is a migraine treated?
There isn’t a cure for migraines. But a healthcare provider can help you manage migraine symptoms through the following:
- Taking medications.
- Avoiding migraine triggers.
- Using alternative migraine remedies.
What medications treat migraines?
A healthcare provider might recommend taking medications to treat migraines. There are two types of medications available:
- Medications to stop migraines: You can take these medications at the first sign of a migraine. They stop or reduce migraine symptoms like pain, nausea, sensitivity, and more.
- Medications to prevent migraines: A healthcare provider usually prescribes preventive medications if you experience severe symptoms that interfere with your routine or have frequent migraines. These medications reduce how often and how severe migraines affect you. You can take these medications as directed, usually daily.
Common medications that stop migraines include:
- Triptans (5-hydroxytryptamine).
- Ditans (lasmiditan).
- Gepants (rimegepant and ubrogepant).
- Dihydroergotamine (prochlorperazine).
- Antiemetic medications (metoclopramide).
Common preventive migraine medications include:
- Antiseizure medications (valproic acid, topiramate).
- Beta-blockers (atenolol, propranolol, nadolol).
- Calcium channel blockers (verapamil).
- Monoclonal antibodies(erenumab, fremanezumab, galcanezumab).
- Tricyclic antidepressants (amitriptyline, nortriptyline, doxepin).
- Serotonin and norepinephrine reuptake inhibitors (venlafaxine, duloxetine).
Medications come in different forms, like:
- An injection under your skin (subcutaneous).
- An oral medication (taken by mouth).
- A nasal spray.
- Through an IV (intravenously).
- Suppository.
You and your healthcare provider will discuss the specific medication, combination of medications, and formulations to best manage your symptoms. All medications should be used under the direction of a headache specialist or provider. As with any medication, it’s important to carefully follow your provider’s instructions.
Over-the-counter migraine medications
Over-the-counter migraine medications are effective if you have mild to moderate migraine symptoms. The main ingredients in pain-relieving medications are ibuprofen, aspirin, acetaminophen, naproxen and caffeine.
Be cautious when taking over-the-counter pain relievers. Sometimes, overusing them can cause analgesic-rebound headaches or a dependency problem. If you’re taking any over-the-counter pain medications more than two to three times a week, let your healthcare provider know. They may suggest more effective prescription medications.
Avoiding migraine triggers
A healthcare provider can help you identify what triggers your migraines. They may ask you to keep a migraine journal or diary. A migraine journal can help you keep track of when a migraine happened, how you felt, and how long it lasted. You can also add details about the foods you ate or the activities you participated in to learn more about any possible triggers.
There are some smartphone apps available to help you keep a migraine journal.
Once you identify a trigger, you can take steps to avoid it. This isn’t always possible, but awareness of your triggers is helpful to identify them and treat a migraine when it starts.
For example, if stress is a trigger, you may want to speak with a mental health professional to help you manage your stress. If you get migraine symptoms when you miss a meal, set an alarm on your phone to remind you to eat meals on a regular schedule.
Alternative migraine remedies
You may want to try alternative therapies to help you manage migraines. These include:
- Taking vitamins, minerals or herbs like riboflavin (vitamin B2), magnesium, feverfew, butterbur or co-enzyme Q10.
- Relaxation techniques like yoga.
- Acupuncture.
- Biofeedback.
- Botulinum toxin type A injections (Botox®).
Talk to your healthcare provider before starting any alternative therapies for migraines.
What migraine treatments are available during pregnancy?
Talk to your healthcare provider if you’re pregnant or plan on becoming pregnant and experiencing migraines. Your provider might suggest avoiding medications for migraines when you’re pregnant or if you think you may be pregnant. Some medications can negatively affect the fetus’s development.
Your provider can recommend alternative treatment options like an acetaminophen pain reliever for migraines.
How do I deal with a migraine as it happens?
There are certain things you can do to help you feel better when a migraine attack happens, including:
- Resting in a dark, quiet, cool room.
- Apply a cold or warm compress or washcloth to your forehead or behind your neck.
- Massaging your scalp.
- Applying pressure to your temples in a circular motion.
- Keeping yourself in a calm state (meditating).